
INTRODUCTION:
Picture this: a 42-year-old office-goer, rushing through emails on a Monday morning, suddenly clutches his chest. He is fit-looking, does not smoke, and has no obvious warning signs. Yet within minutes, he is rushed to the hospital with a heart attack.
This is no longer rare; it is becoming the story of modern India. Every year, nearly 15 lakh Indians die from heart attacks, and more than six crores live with heart disease. What is even more troubling is how young we are when it strikes. Indians face heart disease 10-15 years earlier than people in the West, often right in the middle of careers, families, and responsibilities.
How does a heart issue start?
At the core of most heart attacks and strokes is a process called Atherosclerosis. Think of your arteries as flexible pipes carrying blood to every organ. Over time, these pipes can get lined with fatty deposits called plaque. This plaque is made of cholesterol, triglycerides, calcium, and dead immune cells.
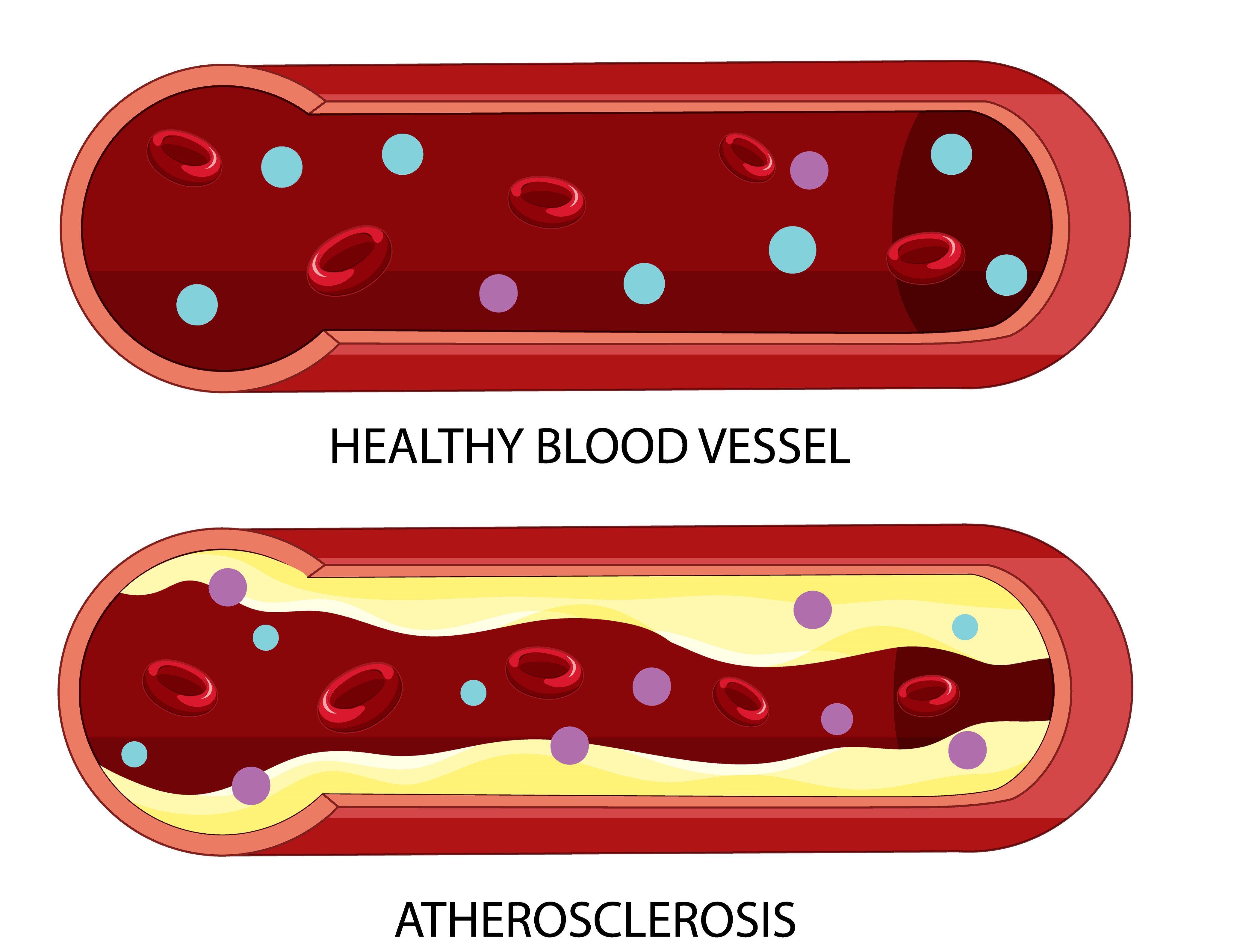
At first, the buildup is silent; you will not feel anything. But as the plaque grows, it narrows the artery, making it more difficult for blood to reach vital organs, such as the heart and brain. Worse still, if a piece of plaque suddenly ruptures, it can trigger a blood clot that completely blocks the artery. When this happens in the heart, it causes a heart attack. In the brain, it causes a stroke.
LIPOPROTEINS
Lipoproteins are special fat-protein complexes that act as transport vehicles in your bloodstream. They transport cholesterol, triglycerides, and fat-soluble vitamins, such as A, D, E, and K, to various parts of the body.
But why do fats even need these carriers? The answer lies in chemistry: fats are not water-soluble, and your blood is mostly water. Without a transport system, fats would float around uselessly, unable to reach the cells that depend on them.
Lipoproteins, like cargo ships, play a vital role in maintaining your body’s functions. They safely package fats, load them onto the cells that need fuel for energy, raw materials for hormone production, or building blocks for cell repair.
There are many types of lipoproteins, but two play the starring roles in heart health:
LDL (Low-Density Lipoprotein) – often labelled as the “bad” cholesterol because, in excess, it can get stuck in arteries and cause damage.
HDL (High-Density Lipoprotein) – often called the “good” cholesterol because it clears out excess cholesterol, returning it to the liver for disposal.
The delicate balance between LDL and HDL is a key factor in heart health. When this balance tips too much toward LDL and too little HDL, the risk of atherosclerosis increases, underscoring the importance of a balanced diet and lifestyle.
What’s inside LDL?
Each LDL particle is like a tiny delivery truck. Inside, it carries:
- One ApoB protein, this works like the truck’s license plate, tagging it so it can bind to receptors and drop off its cargo.
- Cholesterol esters and triglycerides are the actual goods being delivered.
- A surface made of phospholipids and free cholesterol, the outer shell that keeps the package stable while it travels.
Here is the catch: it is not just how much cholesterol these trucks are carrying that matters. What really counts is how many trucks are on the road at once. Each LDL particle carries one ApoB protein, so ApoB acts like a headcount. The higher your ApoB, the more LDL particles are circulating, and the more likely some of them are to crash into the artery wall and cause damage.
LDL vs HDL – What’s the key difference?
LDL and HDL play opposite roles in cholesterol transport.
LDL’s job is to deliver cholesterol to tissues, which is vital for normal body function. Your cells require it for hormone production, maintaining membrane structure, and cellular repair. The problem starts when LDL levels are too high. Extra LDL can become trapped in the walls of arteries, triggering the chain reaction that leads to plaque buildup and heart disease.
HDL, in contrast, acts like the cleanup crew. It removes excess cholesterol from tissues and artery walls, carrying it back to the liver for disposal. This protective role is one reason higher HDL levels are generally linked with lower risk of Atherosclerosis.
But here is the real twist: what matters most is not just your “cholesterol level.” For decades, total cholesterol or LDL-C (the total amount of cholesterol carried by LDL particles) was the standard marker. The problem? It does not always tell the whole story.
Each LDL particle carries one ApoB protein, which makes ApoB a direct measure of how many LDL particles are circulating in your blood. More particles mean more risk of damage, even if the total amount of cholesterol (LDL-C) looks “normal.”
That is why advanced lipid testing is worth asking about. ApoB levels, or LDL particle number, are far more accurate predictors of heart disease risk than total cholesterol alone. You could have a “normal” LDL-C on paper, but still face high risk if your ApoB count is elevated.
How does Atherosclerosis develop?
When too many LDL particles are floating around in your blood, some of them start sneaking into the inner lining of your arteries (called the endothelium). This is more likely if the lining is already weakened by high blood pressure, smoking, diabetes, or chronic stress.
Once LDL particles enter, they do not simply sit there quietly. They undergo oxidation, essentially becoming “rancid.” This oxidised LDL sets off alarm bells in your immune system.
Macrophages, a type of immune cell, rush to the scene like cleanup crews. They swallow up the oxidised LDL, but in the process, they transform into what are called foam cells. These foam cells eventually die and pile up, leaving behind fatty debris.
To contain the mess, smooth muscle cells in the artery wall build a fibrous cap over the area and deposit calcium. This combination of fat, dead cells, and scar tissue is known as plaque.
Over time, this plaque thickens and hardens, gradually narrowing the arteries. Less space means less blood can flow to vital organs, such as the heart and brain. If a plaque ruptures suddenly, it can form a blood clot that completely blocks the artery, triggering a heart attack or stroke.
What about triglycerides?
Yes, high triglycerides also contribute to Atherosclerosis, especially when combined with low HDL and small, dense LDL particles.
- Elevated triglycerides are often a sign of insulin resistance or poor metabolic health.
- They promote the formation of remnant lipoproteins, which are also ApoB-containing particles and atherogenic.
- High triglycerides can lower HDL and promote inflammatory responses in the vessel walls.
So, while LDL remains the central driver, elevated triglycerides also play a meaningful role in cardiovascular risk.
Who’s most at risk?
- People with high LDL or ApoB levels.
- Those with obesity, insulin resistance, or a sedentary lifestyle.
- Individuals with high blood pressure, type 2 diabetes, or who smoke.
- People with a diet high in saturated fats, sugar, or processed foods.
- Those with chronic stress or poor sleep hygiene.
A significant risk factor often overlooked: Family History
If a parent or sibling had heart disease before age 55 (men) or 65 (women), your risk goes up by 2 to 5 times.
You may inherit:
- Higher baseline LDL or ApoB levels
- Genetic mutations (e.g., familial hypercholesterolemia)
- Greater tendency toward inflammation or blood clotting
Knowing your family history is as important as knowing your cholesterol numbers.
How to Manage this?
The good news is that you can actively lower your ApoB levels, strengthen your arteries, and protect your heart with practical lifestyle changes.
✅ Limit saturated fats (like fatty meat, butter, and excess ghee).
Why the caution about ghee? While small amounts are acceptable, excessive saturated fat increases the number of LDL particles, particularly in individuals with a genetic predisposition to high cholesterol levels. Extra spoonfuls of ghee, often seen as “healthy tradition,” can backfire, particularly if your daily routine is mostly sedentary.
✅ Load up on heart-friendly foods: fruits, vegetables, whole grains, legumes, lean proteins, and nuts. These provide fibre, antioxidants, and nutrients that help balance cholesterol and support vascular health.
✅ Cut down on refined carbs and added sugars. They drive insulin resistance, raise triglycerides, and worsen the cholesterol mix that clogs arteries.
✅ Exercise regularly, aim for at least 3–4 sessions a week. A combination of cardio (for endurance and circulation) and resistance training (for muscle development and metabolism) is the most effective approach.
✅ Lose 5–10% of body weight if you’re overweight. Even modest weight loss can significantly improve lipid levels and reduce the risk of cardiovascular disease.
✅ Quit smoking and moderate alcohol. Smoking directly damages the endothelium (artery lining), while heavy drinking worsens blood pressure and triglycerides.
✅ Manage stress and sleep better. Poor sleep, chronic stress, and burnout are silent contributors to heart disease. Mindfulness, relaxation, and active recovery aren’t luxuries; they’re protective habits.
These small, consistent steps act like turning down the speed of plaque buildup. They won’t just add years to your life; they’ll add quality to those years.
Conclusion
Heart disease doesn’t appear out of nowhere; it builds silently over years through excess LDL particles, rising ApoB levels, and everyday habits that go unchecked. The tragedy is that for many Indians, the first symptom is often the heart attack itself.
But here’s the hopeful part: you’re not powerless. By paying attention to ApoB and undergoing advanced lipid testing, and making thoughtful changes to your diet, Exercise, sleep, and stress management, you can take control of your cardiovascular health long before a crisis strikes.
Your arteries are highways that carry life itself. Keep them clear, keep them strong, and they’ll take you far. The best time to act was yesterday; the next best time is today.
FAQs on Heart Health and ApoB
- If my cholesterol levels are normal, should I still be concerned?
Yes. Normal LDL-C doesn’t always mean low risk. High ApoB (particle count) can still contribute to plaque buildup even if cholesterol levels appear normal.
- What is ApoB, and why does it matter?
ApoB is a protein on LDL particles. Each LDL particle contains one ApoB, which indicates the number of particles circulating; a higher ApoB level equals a higher risk of heart disease.
- Is all LDL bad?
No. LDL is essential for hormone production and cell repair. The danger comes when there’s too much, leading to artery blockages.
- Why do triglycerides matter?
High triglycerides signal poor metabolic health. They lower HDL levels, worsen LDL quality, and accelerate the formation of plaque.
- Is ghee harmful for the heart?
In moderation, no. However, excess ghee, especially in sedentary lifestyles, can increase the LDL particle count and raise the risk.
- Can family history be overcome?
Yes. Genetics raises the baseline risk, but diet, Exercise, stress management, and tests like ApoB can significantly reduce your chances.
- How much Exercise protects the heart?
At least 150 minutes of cardio per week, plus two resistance training sessions, helps keep your arteries and heart stronger.




